Curriculum & Educational Program Objectives

The Roseman Readiness Curriculum
The practice of medicine changes rapidly. Physicians increasingly need to understand social determinants of health, interface with emerging technology, manage knowledge streams, work in interprofessional teams and health systems, and communicate complex, personalized information to patients and families.
Our students will be ready.
The Roseman Readiness Curriculum is a highly integrated curriculum that emphasizes patient care in the setting of today’s advances. Diagnostic and therapeutic skills are taught from the beginning of the curriculum in the context of foundational basic and health systems sciences, with a focus on ethical principles, professionalism, and societal context. Students train to communicate flexibly, authentically, and respectfully with patients, caregivers, colleagues, and other healthcare team members to navigate a changing world effectively.
The Roseman Readiness Curriculum is competency-based and delivered in active learning formats that require students to take charge of their own learning and become lifelong learners. Groups of households in GENESIS, Roseman’s household-centered care delivery model, are managed as practices by students working with faculty physicians and interprofessional teams, merging student learning with service to the community and allowing value-based metrics to influence decision-making.
The future of medical education is at Roseman!
Curriculum & Educational Program Objectives
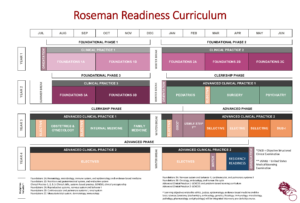
The general structure of the curriculum includes an 18-month pre-clerkship phase, followed by a 12-month clerkship phase, and a subsequent advanced phase that continues to graduation.
The pre-clerkship curriculum is structured as an integrated, one-pass curriculum delivered in three phases – Foundational Phases 1, 2, and 3. Within these phases, course blocks of 6-8 weeks cover integrated basic science, organ systems, clinical science, biomedical ethics, and health systems science content. Each week includes approximately 25 hours of assigned time, including preparatory time for class sessions. Basic science, clinical science, and health systems science content is stratified across clinical/organ systems-focused blocks and mapped both to ensure coverage of all learning objectives and to avoid gaps and redundancies.
Each foundational phase also contains a longitudinal Clinical Practice course (Clinical Practice 1, 2, and 3) that integrates clinical skills education and RUCOM’s experiential clinical and service-learning curricular component, part of the GENESIS household-centered care program, as well as a clinical preceptorship experience. Through GENESIS, all students will work with assigned households to provide household-centered care and home visits. Grouping these households into practices that are aligned with student learning communities will allow for real-life exposure to population health and practice management. Foundational Phases 1 and 2 also incorporate a preceptorship experience that provides students with early exposure to practicing clinicians in the local community.
The Clinical Practice course content is delivered through dedicated focus weeks that allow for concentrated practice of clinical skills and through one half-day per week assigned to GENESIS participation, early experiential exposure to patient care, and systems-based practice content. Dedicated RUCOM physician faculty members provide both clinical skills training and GENESIS household-centered care supervision. RUCOM’s learning community structure provides the organizational basis for participation in GENESIS.
Along with physicians, outreach workers are assigned to each learning community. Outreach workers recruit and manage individual households and maintain relationships with the community partners that serve as referral sources. GENESIS has recruited over 140 households and involved more than 75 community partners.
| Pre-Clerkship Course Name: | Disciplines Included*: |
| Foundations 1A | Hematology, microbiology, immune system, epidemiology and evidence-based medicine |
| Foundations 1B | Nutrition and gastrointestinal system, and endocrine system |
| Clinical Practice 1 | Clinical skills, systems-based practice, GENESIS |
| Foundations 2A | Reproductive system, nervous system and behavior I |
| Foundations 2B | Cardiovascular and pulmonary systems I, renal system |
| Foundations 2C | Musculoskeletal system, dermatology, immunology |
| Clinical Practice 2 | Clinical skills, systems-based practice, GENESIS |
| Foundations 3A | Nervous system and behavior II, cardiovascular and pulmonary systems II |
| Foundations 3B | Oncology, embryology, human life cycle |
| Clinical Practice 3 | Clinical skills, systems-based practice, GENESIS |
*Learning objectives related to ethics and justice will be integrated into every pre-clerkship course.
The clerkship phase includes six mandatory clerkships, two of which have eight weeks of clinical time (Internal Medicine and Surgery), and four of which have six weeks of clinical time (Obstetrics and Gynecology, Psychiatry, Pediatrics, and Family Medicine). Each clerkship also has an introductory week focused on clerkship-specific didactics to allow for adequate clerkship preparation. In addition, students have five weeks of elective time in the clerkship phase of the curriculum, in which they can choose from a list of specialty rotations that they wish to explore prior to the advanced phase. A longitudinal course, Advanced Clinical Practice 1, will run the length of the clerkship year, bringing all clerkship students back to campus for problem-based learning sessions and GENESIS curricular experiences.
At the end of the clerkship phase, students have a promotional OSCE followed by dedicated study time for USMLE Step 1. Students are required to take Step 1 prior to entering the advanced phase and must earn a passing score to continue. The advanced phase consists of a sub-internship as well as required selective and elective rotations. Students must take USMLE Step 2 by September of the advanced phase. A longitudinal course, Advanced Clinical Practice 2, will allow for continuity with GENESIS households and practice management. The month-long Advanced Clinical Education and Simulation course at the end of the advanced phase allows for final preparation for entering residency.
Roseman University College of Medicine Competency Domains and Medical Educational Program Objectives. Note that all competencies are framed so that determination of achievement of a level of competence is appropriate for the student’s level of training.
| Competency Domain | Competencies/EPOs |
| Patient Care (PC): Provide patient-centered care that is compassionate, appropriate, and effective for the treatment of health problems, prevention of disease, and the promotion of health. | Perform all technical procedures-medical, diagnostic, and surgical-considered essential. (PC 1) |
| Gather essential and accurate information about patients and their conditions through history-taking, physical examination, and the use of laboratory data, imaging, and other tests. (PC 2) | |
| Apply the concepts and principles of patient safety science in the delivery of clinical care. (PC 3) | |
| Appropriately interpret laboratory data, imaging studies, and other tests required for the area of practice. (PC 4) | |
| Formulate diagnostic evaluation, therapeutic interventions, and patient management plans based on patient information and preferences, up-to-date scientific evidence, and clinical judgment. (PC 5) | |
| Counsel and educate patients and their families to empower them to participate in their care and enable shared decision making. (PC 6) | |
| Understand the need, value, and processes of consultations and referrals in the delivery of health care, the monitoring of patient progress and outcomes, and the management of continuity of care. (PC 7) | |
| Apply preventive and health maintenance principles and techniques as appropriate to the clinical context in the delivery of healthcare. (PC 8) | |
| Exhibit appropriate role modeling and provide supervisory responsibilities commensurate with one’s level, abilities, and qualifications. (PC 9) | |
| Knowledge for Practice (KP): Demonstrate knowledge of established and evolving biomedical,
clinical, epidemiological, and social-behavioral sciences, as well as the application of this knowledge to patient care. |
Demonstrate an investigative and analytic approach to clinical situations. (KP 1) |
| Apply established and emerging biomedical scientific principles fundamental to health care for patients and populations. (KP 2) | |
| Apply established and emerging principles of clinical sciences to diagnostic and therapeutic decision-making, clinical problem-solving, and other aspects of evidence-based health care. (KP 3) | |
| Apply principles of epidemiological sciences to the identification of health problems, risk factors, treatment strategies, resources, and disease prevention/health promotion efforts for patients and populations. (KP 4) | |
| Apply principles of social-behavioral sciences to provision of patient care, including assessment of the impact of psychosocial-cultural influences on health, disease, care-seeking, care compliance, and barriers to and attitudes toward care. (KP 5) | |
| Demonstrate an understanding of the creation, dissemination, and translation of new health care knowledge and practices. (KP 6) | |
| Self-Assessment and Adaptive Learning (SAL): Demonstrate the ability to identify knowledge gaps, to develop a personal learning plan, to evaluate one’s care of patients, and to appraise and assimilate scientific evidence. | Identify strengths, deficiencies, and limits in one’s knowledge and expertise. (SAL 1) |
| Set short-term and intermediate learning and improvement goals. (SAL 2) | |
| Identify and act upon one’s gaps in knowledge, skills, or attitudes. (SAL 3) | |
| Systematically analyze clinical scenarios using quality-improvement methods and recommend changes with the goal of practice improvement. (SAL 4) | |
| Seek and incorporate formative feedback. (SAL 5) | |
| Locate, appraise, and assimilate evidence from relevant and current scientific studies to inform clinical decisions. (SAL 6) | |
| Use information technology to optimize learning and improve patient care. (SAL 7) | |
| Participate in the education of patients, families, students, trainees, peers, and other health professionals. (SAL 8) | |
| Obtain and utilize information about individual patients, populations of patients, or communities from which patients are drawn to improve care. (SAL 9) | |
| Interpersonal and Communication Skills (ICS): Demonstrate interpersonal and communication
skills that result in the effective exchange of information and collaboration with patients, their families and support networks, and health professionals. |
Engage in practices that promote inclusive and collaborative communication with patients, families, and others as appropriate across a broad range of backgrounds and experiences. (ICS 1) |
| Communicate effectively with colleagues within one’s profession or specialty, other health professionals, and health related agencies. (ICS 2) | |
| Work effectively with diverse individuals as a member of a health care team or other professional group. (ICS 3) | |
| Act in a consultative role to other health professionals. (ICS 4) | |
| Demonstrate the ability to produce professional, comprehensive, timely, and legible medical documentation. (ICS 5) | |
| Demonstrate sensitivity, honesty, and compassion in difficult conversations, (e.g., about death/end-of-life, other “bad” news, adverse events, disclosure of errors, sexuality, substance use, mental and behavioral health, and other sensitive topics). (ICS 6) | |
| Demonstrate insight and understanding about emotions and human responses to emotions that allow one to develop and manage interpersonal interactions. (ICS 7) | |
| Professionalism (P): Demonstrate interpersonal and communication
skills that result in the effective exchange of information and collaboration with patients, their families, and health professionals. |
Demonstrate compassion, integrity, and respect for persons. (P 1) |
| Demonstrate responsiveness to patient needs that supersedes self-interest. (P 2) | |
| Demonstrate respect for human dignity, confidentiality, privacy, autonomy, and informed choice. (P 3) | |
| Fulfill obligations to fellow students, patients, society, and the profession. (P 4) | |
| Demonstrate awareness of and responsiveness to diverse patient populations, including but not limited to diversity in gender, sex, socioeconomic status, age, culture, race, religion, disability, and sexual orientation. (P 5) | |
| Demonstrate a commitment to ethical principles pertaining to provision or withholding of care; public health; research; and business practices, including compliance with relevant laws, policies, and regulations. (P 6) | |
| Systems-Based Practice (SBP): Demonstrate an awareness of and responsiveness to the larger context and system of health care, as well as the ability to call effectively on other resources in the system to provide optimal health care.
|
Work effectively in various health care delivery settings and systems. (SBP 1) |
| Participate in the coordination of patient care within the health care system. (SBP 2) | |
| Incorporate considerations of cost awareness and risk-benefit analysis in patient and/or population-based care. (SBP 3) | |
| Advocate for quality patient care and optimal patient care systems. (SBP 4) | |
| Participate in identifying system errors and implementing potential systems solutions. (SBP 5) | |
| Participate in administrative and practice management activities commensurate with one’s role, abilities, and qualifications. (SBP 6) | |
| Interprofessional Collaboration (IPC): Demonstrate the ability to engage in an interprofessional
team in a manner that optimizes safe, effective patient- and population-centered care.
|
Work with other health professionals to establish and maintain a climate of mutual respect, dignity, diversity, ethical integrity, and trust. (IPC 1) |
| Use the knowledge of one’s own role and the roles of other health professionals to appropriately assess and address the health care needs of the patients and populations served. (IPC 2) | |
| Communicate with other health professionals in a responsive and responsible manner that supports the maintenance of health and the treatment of disease in individual patients and populations. (IPC 3) | |
| Participate in interprofessional teams to establish, develop, and continuously enhance patient- and population-centered care that is safe, timely, efficient, effective, and equitable. (IPC 4) | |
| Professional Identity Formation (PIF): Demonstrate the qualities required to sustain
lifelong personal and professional growth as a physician. |
Develop the ability to use self-awareness of knowledge, skills, and emotional limitations to engage in appropriate help-seeking behaviors. (PIF 1) |
| Demonstrate knowledge of healthy coping mechanisms to respond to stress. (PIF 2) | |
| Demonstrate awareness of potential for conflicts between personal and professional responsibilities and knowledge of support resources. (PIF 3) | |
| Demonstrate responsiveness to feedback in a professional manner. (PIF 4) | |
| Demonstrate trustworthiness that makes colleagues feel secure when one is responsible for the care of patients. (PIF 5) | |
| Provide leadership skills that enhance team functioning, the learning environment, and/or the health care delivery system. (PIF 6) | |
| Demonstrate appropriate self-confidence that puts patients, families, and members of the health care team at ease. (PIF 7) | |
| Recognize that ambiguity is part of clinical health care and respond by utilizing appropriate resources in dealing with uncertainty. (PIF 8) |